The Best iPad EMR Software and Buyer's Guide 2025
Emiley Parker
Emiley Parker
Apple iPads are becoming quite famous in the healthcare industry. Its sleek design, beautiful user interface, and long battery life have attracted many physicians. Due to the increased popularity of iPads among physicians, EMR software vendors are now developing EHR software that offers complete accessibility on iPads. Some vendors offer Native iPad apps and some offer accessibility through web browsers.
There are three major types of iPad EMR Software which are listed below:
Web-based iPad EMR Software - These types of iPad EMRs can be accessed through web browsers on iPads. The software can also be accessed through the iPad’s native web browser i.e. Safari.
Native iPad EMR Software - This is the most famous type of iPad EMR software. It is an app that is specifically developed for iPads and works amazingly on iPads. But the options on Native iPad EMR software are very limited as of now. But the constant version updates are bringing improvements gradually.
Remote-access EMR Software - Remote-access EHR software is on-premise EMRs that can be accessed through a remote system like iPads using utilities such as Citrix. It is not a very common type of iPad EHR software but it works. Remote access EHR allows users to view the software as if the user was using a desktop or laptop.
Before choosing an iPad EMR Software, you should make sure the software has the following key features:
Appointment Scheduling – iPad EHR Software must allow medical professionals to view and manage their schedules directly from their iPads. The scheduling feature can be used by both patients and doctors to find free appointment slots, specify clinic locations and manage clinic capacity. The software must also offer the functionality to add and edit appointments, manage multiple locations and create schedules for single or multiple providers.
Data Documentation – We all know that healthcare practices need to maintain a large volume of documents. iPad EMR software should offer a data management feature that can help manage EMRs and images and reduce records retention costs. The software must also provide electronic document storage and management features to eliminate the need for an off-site storage facility. The iPad app should be able to handle multiple file types and may also offer document scanning capabilities.
HIPAA Compliance – Before implementing an iPad EMR software, you should make sure that it is compliant with all HIPAA regulations and has all the latest updates.
Appointment Alerts & Reminders – The top iPad EHR software must be able to send appointment reminders to patients via text messages or email. This saves a lot of time and automates the routine tasks of sending appointment alerts and reminders to patients. This also reduces the risks of no-shows.
e-Prescribing (e-Rx) – The iPad EHR Software must offer an e-Prescribing (e-Rx) feature. e-Prescribing (e-Rx) reduces medication errors, reviews previous prescriptions, searches for pharmacy locations, and provides alerts regarding drug allergies, dosage levels, and duplicates. It also allows physicians to create and refill prescriptions, view dosage history, contact pharmacies and manage medications.Electronic Medical Records Software or commonly referred to as EMR Software represents the electronic method of storing medical records for patients. Using specially designed software, physicians and other medical professionals can store anything ranging from patient demographics to extensive clinical information about patients, such as medical history, social history, lab reports, and more.
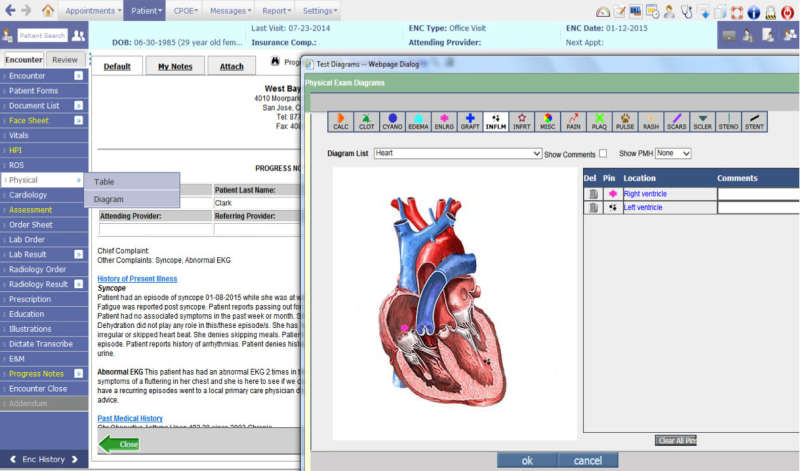
Since all medical providers (MDs, DOs, PAs, NPs, LCSW, OT, etc.) work distinctly based on their background and medical specialty, EMR Software or EHR Software must accommodate the unique style and documentation requirements. Examples of such specialty-specific features include the ability to annotate images or the capability to store before/after photos for Pain Management specialists and Dermatology specialists respectively. Similarly, other specialties such as Pediatrics, Oncology, Podiatry, Ophthalmology, Neurology, Nephrology, Dialysis Centers, Rheumatology, and Chiropractic Care require their unique set of specialty-specific features to simplify adoption.
Since the introduction of the HITECH Act, healthcare IT has undergone a massive transition starting from the widely recognized Meaningful Use program to what is now known as MACRA, the Medicare EHR Incentive Program. The Meaningful Use program has transformed and now formed part of the four components of the new Merit-Based Incentive Payment System (MIPS), which itself is a fundamental part of MACRA.
For some medical practices, the transition from paper-based records to EMR Software (Electronic Medical Records Software) has not been a simple one. Regardless, realizing that the benefits of utilizing ONC Certified EMR Software far outweigh the hassle and challenges associated with it - ensuring a viable future, most practices today have successfully transformed their clinical and administrative operations to EMR Software.
Aside from ensuring tangible financial incentives and profitability, practices converting to EMR / EHR Software have seen the following benefits:
Just like a medical specialty, EHR Software requirements also depend on the size of the medical practice. From solo-provider clinics to large multi-provider, multi-specialty clinics, every practice has unique inherent challenges that must be addressed by the EMR Software vendor.
A small doctor’s office not only has a limited number of staff members but their EMR Software budgets are also extremely low compared to a large enterprise such as a hospital. Due to these budgetary constraints, many providers simply choose to employ Free EMR Software or choose an affordable EHR Software vendor with a low fixed monthly fee. Cloud-based access is one such important requirement so that these providers can access patient charts even from home when needed.
These practices usually consist of 5 to 10 medical providers often belonging to the same medical specialty. Their requirements are more stringent, and their budget is also considerably large. Aside from specialty-focused requirements (EHR Software by Specialty), these practices also require unique features such as interoperability, dedicated customer support, multi-device support as well as extensive reporting functionality to keep an eye on the overall performance of the practice.
Larger group practices generally comprise more than fifteen or often twenty medical providers. These practices usually provide medical services that fall under various medical specialties (Orthopedics, Pain Management, Surgery, Chiropractic Medicine, Family Medicine, etc.). Therefore, these practices require support for multiple users to access the system simultaneously, as well as for the Scheduling software to accommodate multiple locations, providers, and resources such as Dialysis Chairs, procedure room allocation, etc. These practices also keep replacing or adding staff members and need a scalable solution.
EHR software companies such as Epic, Cerner, AllScripts, NextGen, Athenahealth, IMS by Meditab, eClinicalWorks, Meditech, McKesson, MEDHOST, etc. usually target and provide solutions for larger corporations like Hospitals, ACOs, PCMH, IPAs, CINs (Clinically Integrated Networks), Public Health Departments, etc.
These customers have the most elaborate list of requirements, which are usually documented in the form of an RFI or RFP to assess and shortlist vendors that can meet them. The requirements consist of features like inventory management modules, interface with local labs (LIS), machines, and diagnostic equipment along with drug dispensing (pharmacy management software) and electronic medication administration records (EMAR), etc.
These entities also require the EHR software also need to integrate with multiple other software and medical devices.
Since the introduction of Meaningful Use, most healthcare practices simply have little or no choice but to convert their practice operations to EHR software. However, most providers today select the EHR software of their choice that best suits their specific needs and must perform an extensive search to evaluate all available options before they find one that is suitable. Most potential EMR Software buyers in the market today have the following in common:
Although #3 is ideal, every provider and their practice workflows are unique and therefore what works for one provider may not suit the other. “One size fits all” simply doesn’t apply in the world of healthcare IT. Software experts and industry specialists are an ideal source of information, advice and ultimately ensure that the right decision is made.
EMR software includes several types of software based on specific applications or functionalities:
Small doctor offices benefit the most from Cloud-based EMR Software technology since minimum to no upfront cost or maintenance is required and accessing the EHR Software is possible from any location given the availability of internet access. This type of EMR software is also device independent in most cases and can be accessed using devices such as Smartphones (Android & iOS), iPhones, iPads, laptops, and desktop computers.
Apple dominates the digital device and computer market in the US today, so it is no surprise that many providers are specifically looking for their EMR Software vendor to support Mac operating system (Mac EMR Software). Not all Vendors today work on a Mac device, so looking for a vendor with native support for Mac devices is essential to ensure that the software performs on existing hardware at the practice and does not require more investment in computer systems.
This is the most significant requirement for most software buyers today as the software must comply with the standards and guidelines set by the Office of the National Coordinator (ONC). The online repository details all software vendors and details related to their respective compliance with the measures set by the ONC (Click here). Software that complies with these standards has undergone rigorous testing and confirmed at a benchmark level defined by the federal body. The software testing done during this exercise checks all areas of the EMR Software system from Patient Portal access to the way the EHR Software communicates with other programs and entities like labs, Pharmacies (via e-Rx), hospitals, HIEs, etc.
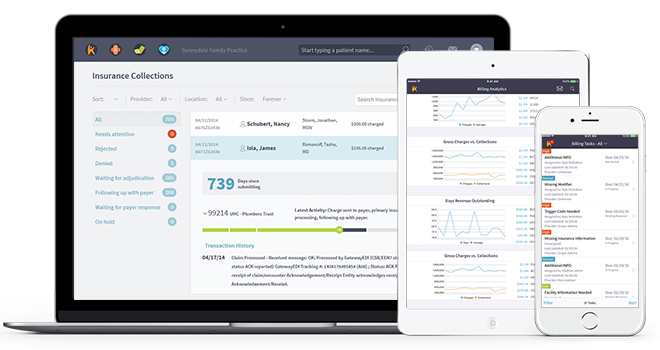
With competition rising in healthcare IT, EMR software providing integrated Practice Management software as part of their overall software package easily outperform rivals with standalone EHR Software including those that may provide specialty-specific EHR software. EMR Software companies with integrated Practice Management solutions often tend to provide extensive reporting capabilities to track practice performance and manage business operations better.
Medical practice has several needs of software systems to streamline operations across the board. One such important area is billing for services rendered and communications with insurance companies. Medical Billing Software, therefore, works best when integrated with Electronic Health Records software. All clinical documentation seamlessly conforms to the required standard and forms a financial document that can be electronically sent to payers (insurance carriers) to verify and process at their end. This simplifies the operations and ensures all parties are on the same page when it comes to the financial health of the enterprise. Medical billing software helps practices and medical billing managers generate claims, patient statements, verify patient eligibility, and more. This software is ideal for practices that want to handle billing in-house and can integrate with EMRs.
An EMR Software must ensure the security and safety of patient records while ensuring privacy and HIPAA compliance for patient/doctor communication (Patient Portal). This is a paramount concern for physicians and HIPAA compliance should be guaranteed at all times by the EHR Vendor. Most Vendors today (Epic, Cerner, Athenahealth, AdvancedMD, PrognoCIS, Modernizing Medicine, eClincalWorks, etc.) are aware of the importance of HIPAA compliance and have taken steps to ensure the safety of patient records security in every section of the EHR Software using advanced tools like data encryption technologies to enhance the security of the EMR software.
One of the decisions your practice will have to make is whether you want just EMR software or one with integrated Practice Management for billing and scheduling. There are advantages to having both together but there have been cases where some practices only go for one if they had unique requirements that a vendor could not fulfill, or they had already paid a hefty amount for PM software and weren't looking to replace it yet.
Doctors are not IT professionals, and though some might be tech-savvy, it would be egregious to expect them all to be experts on EHR software. Ease of use is essential to make the transition from paper to electronic smooth, as well as day-to-day practice to go along without a hitch. If the software is too complicated and hard to understand, it's a waste of precious time and needlessly aggravating. Some vendors offer free training while others don't; make sure you ask for training if your practice needs it.
Not all specialties are created equal, so why must their software be generic? Basic EHR software works well and is good for general practice and most specialties, but doctors have complained about specialty specific not being available in the market. The specialty software has inbuilt recording systems that make specialty practices function efficiently. Only a few vendors provide specialty-specific software, so there aren't many to choose from. But more vendors are cottoning on to the demand and there should be more options in the near future.
Support is a major issue most practices have with their current vendors. A good support team can make small glitches to major roadblocks easy to maneuver while a bad one will just make things worse. Some vendors provide support as part of the plan you're already paying for, while others charge extra for support. Scout the market, read reviews, or just ask point-blank if there will be a special support team assigned to each practitioner and whether you'll be charged for the service.
There are varying price lists out there, some offer free services, while others charge an arm and a leg for specialty services. Either way there will be hidden costs that you might get to know about later. Fix your budget and talk to vendors you interview about hidden costs within the contract and whether services such as training and support are free.
Smartphones have changed the dynamics of mobile usage. Handheld devices are easy to carry around and can be used for any number of uses. Most people are ditching the cumbersome PC for a handheld device. Doctors mostly use iPads or Tablets in the examination room to take down patient symptoms, check the history and note down the prescription, so the vendor must have a mobile application that is synced with all the mobile devices being used in the practice.
Like anything else, the EMR software industry is also subject to constant changes. From new technology to legalities and governing bodies, everything is constantly changing. Here are some of the changes I think it would do well for you to keep track of.
Previously at a health care conference Andy Slavitt, the administrator of the Centers for Medicare & Medicaid Services had declared that Meaningful Use was to be over and be replaced by the end of that year with something better. But a deeper look into the claims revealed that meaningful use was always there, only getting more and more improved.
The new measures aim to make the reporting and benchmark for reaching the required reports much easier and laxer than under Meaningful Use, along with other changes.
As the CMS has officially renamed Meaningful Use to "Promoting Interoperability" as of 2018, it's important to understand its updated principles. Effective interoperability of healthcare data will ensure that electronic health information is shared properly between healthcare and public health partners in the right format and at the right time. Starting in 2022, the CMS requires all eligible healthcare services to implement upgraded versions of EHR software that utilize this updated definition.
In 2024, the demand for EMR software solutions for healthcare practices has continued to rise, with market growth estimated at around 6-7% year-over-year as healthcare providers increasingly prioritize digital transformation and interoperability. This increase is largely driven by the adoption of advanced technologies like AI and cloud computing within these systems, which enhance clinical workflows and patient care. Epic Systems has expanded its dominance, now capturing over 35% of the market, particularly among large multispecialty organizations. Meanwhile, Oracle Health (formerly Cerner) has faced challenges, especially in retaining smaller hospitals, contributing to a slight decline in its market share. Together, major players like Epic, Oracle Health, Meditech and Allscripts account for a significant portion of the EHR market, reflecting the ongoing evolution and consolidation within the industry.
Accessibility
EMR software is quickly widening its range of practice types in order to become more accessible to healthcare services. The amount of people who lack the time and knowledge, who are in health IT, is increasing each year. This makes optimizing these software solutions more difficult as they must now cater to different needs. Douglas W. Bowerman, MD, predicts we will see a “continued trend towards accessibility” in EMRs, both in terms of how we access them – on mobile, for instance – and who can access the software.
Real-time Analytics
Healthcare facilities accumulate massive amounts of patient data. Patient health and financial data let vendors help physicians with Clinical Decision Support (CDS). Leveraging analytics algorithm predictions can solve interoperability-related accessibility issues. Data warehouse development is also an opportunity to ensure more accurate patient data thanks to automation.
Blockchain
Despite being used more for cryptocurrency and a recent surge in NFTs, the blockchain has recently found a place in EHR software. The blockchain allows EHR data to be secured through cryptography, making it available only to those who have access to it in the first place. As an example, the blockchain can validate clinical trial and claims results, track medicine distribution and prevent insurance fraud. Although the usage of blockchain in EHR has only just begun since the start of 2022, it is already being used to secure data and ensure confidentiality.
Patient-Centric Engagement
In order for EMR/EHR companies to continue to grow, it's going to require a lot more than simply using existing technology to diagnose your issues. Ensuring patients have consistent engagement throughout the scheduling process is imperative. One of the best ways to boost patient engagement is by increasing your outreach via different social mediums and making content more easily accessible, through patient communities for example. Giving physicians an insight into their patient's health has become paramount and has recently been utilized by including data from smart devices in patient reports.
Changing Dynamics
Technology is innovating on a daily basis and constantly influences electronic health records. For example, common AI virtual assistants are beginning to assist healthcare services, speeding up the diagnostic process and increasing efficiency. Other tech giants are also entering the healthcare field, such as Apple and Google. With their massive budgets, they have the ability to invest heavily in R&D without taking many risks. They have also already witnessed the issues that arise from the lack of interoperability in current iterations of EMR software and are very unlikely to make the same mistakes. This competition is great for consumers and clinicians as it will force EHR vendors to rapidly modernize their systems with far more regular updates, meaning large-scale changes are on the horizon.
Recent research found that only 25% of practitioners are interested in a web-based model and only 50% are willing to have it as an initial model that eventually transitions to cloud-based. Cloud-based EMR software cuts down on steep upfront costs for client servers and can be hosted on any device that has a web browser. It's no surprise that more and more vendors are transitioning to cloud-based software because the industry demands are changing. The move to the public cloud for healthcare is vital in the current changing landscape. For practices that don't adopt new cloud services, the old inferior feature set coupled with the higher prices will hinder the business dramatically. This gulf between the old software and the new cloud-based software will only grow more exponentially as time goes on.
Standardization
The current standards that regulate EMR are very lax. Vendors end up having to pay millions in settlement fees due to false claims about meaningful use certifications. However, regulations are becoming far stricter and more transparent to prevent incidents like this from happening again. The interface between physicians and medical billing coders will likely become more separate. This is because they both need access to completely unrelated pieces of information, so sharing the same regulations often leads to life-threatening miscommunication.
5G
5G Networks are poised to become the forefront of data communication methods in only a few years. They offer up to 100x the speed of contemporary 4G networks yet may still not integrate properly with the current state of healthcare. As it stands, there are many different formats available that are all competing to become the dominant method for EHR communication. As such, medical records are currently spread amongst these different formats; they are incompatible and so the various EHR systems cannot communicate at all. Until a standard is agreed upon, 5G networks won't be able to bypass the bottleneck created by two opposing systems.
Better Patient Access
Despite promising patients access to medical records, this feature has not materialized on EHR systems as of yet. A study in 2019 found that only 10% of patients who had access to their records online actually accessed them; of them, 63% were encouraged to do so by their healthcare providers. In order to prepare for potential regulatory changes in the future, software developers are updating EHR systems to be easier to navigate and better fit the patient's needs. Practices themselves are also now providing proper guidance and awareness about the importance of regularly checking one's own records in order to familiarize themselves before appointments.
EHR Footprint
EHR systems are the forefront supplier of paper-to-screen technology, so it is imperative for the software to be inclusive of a wide range of digital capabilities. Implementing better use of data liquidity will allow data to be more accessible, increasing the EHR footprint. This can be done without sacrificing the security of the data. Implementing better interoperable solutions will also expand the footprint, allowing healthcare organizations to better access and exchange patient data.
Artificial Intelligence
In recent years, advancements in AI and machine learning have dramatically changed the healthcare industry. As these technologies continue to evolve, they are likely to have a significant impact on the future of EHR (Electronic Health Record) and EMR software. By leveraging AI and machine learning algorithms, EMR systems can become more intuitive and efficient, streamlining clinical workflows and improving patient outcomes. The application of AI and machine learning will also enable EMR systems to provide more personalized and proactive care, by analyzing patient data and identifying potential health issues early on. Additionally, these technologies have the potential to revolutionize clinical research and drug development by providing access to vast amounts of patient data and insights.
Digital Therapeutics
Digital Therapeutics involves software that can behaviorally alter patients and help treat mental conditions through the use of different interventions. Usually, digital therapeutics are used through smartphones and tablets. The software is quickly being integrated into EHR software and they aim to be more patient-centric. As they begin to meet industry requirements, their popularity will continue to rise and clinical trial results will continue to be published in peer-reviews journals.
Reducing Errors
In their current state, EHR and EMR software does not properly address medical error prevention. Previously, illegible handwriting on paper prescriptions was blamed, but over-reliance on computers to supply the correct doses for medication can prove to be equally as dangerous. For example, a 16-year-old patient in 2013 was prescribed 38 tablets of medication, but it turned out to be an overdose for someone of that age. These sorts of errors are far more common than we would like to believe. In the future, EMR and EHR software developers are striving to dramatically reduce these errors by decluttering the physician notification center which could cause less time spent attending to patients. Currently, details such as patient implants may not be added to the system before radiological imaging since EHRs don't actually have a standard place to store notes.
Blockchain
Despite being used more for cryptocurrency and a recent surge in NFTs, the blockchain has recently found a place in EHR software. The blockchain allows EHR data to be secured through cryptography, making it available only to those who have access to it in the first place. As an example, the blockchain can validate clinical trial and claims results, track medicine distribution and prevent insurance fraud. Although the usage of blockchain in EHR has only just begun since the start of 2022, it is already being used to secure data and ensure confidentiality.
Searchability
One of the biggest hassles in dealing with current EMR / EHR software is being able to easily navigate through mountains of data. Despite large leaps in technology in recent years, EMR / EHR software is clearly behind in terms of its ease of use and User Interfaces. Electronic Health Records are designed for easier data access than paper files, and EMR vendors are starting to implement updated iterations of their user interface in their software to better achieve this goal.
Wearable Devices
Largely spearheaded by big tech companies such as Apple, wearable devices are surging in popularity in medical fields - the market is expected to grow 26.8% from 2022 to 2028. The devices have allowed healthcare metrics to become far more accessible and have, in turn, made medical diagnosis simpler. Integrating the data from wearable devices into Electronic Health Records (EHR) has the potential to massive improve patient healthcare. The devices include various different sensors that can track body activity and monitor environmental factors. Currently, they come in many different forms, such as smartwatches, fitness trackers, and specialized apps on mobile phones.
Widespread Interoperability
Electronic Medical Records don't offer patients the ability to access their own records across multiple healthcare organizations due to the lack of data-sharing standards set between different practices. This causes significant problems for patients who receive care from multiple different centers. The issue also makes the diagnosis of patients harder for physicians and healthcare providers. Due to this, EMR/EHR providers are updating their software to include interoperability and integration features to allow data to be shared between these different organizations.
Patient Portal
Patient portals completely eliminate the need for paperwork and the manual retrieval of data. On top of this, medical records can be available on demand by offering a portal that patients themselves can access directly. Having easy access to their data encourages patients to be more involved in their health journey, which eases the medical diagnosis process from healthcare specialists.