Pathology EMR software provides pathologists with a powerful range of capabilities to help them identify illnesses from autopsies and biopsy samples. It streamlines clinical and administrative processes, allowing pathologists to diagnose patients more quickly. However, given the complexity of pathology, an EMR software system may not provide all the capabilities needed to enhance patient care.
Pathology-specific EHR software should have the following key features to provide optimal benefit to pathologists:
There are a few factors to consider before selecting a pathology EMR software vendor. These will help your decision-making process:
What is Electronic Health Records (EHR) Software?
Finding Electronic Medical Records (EMR) Software is a time-consuming project. With over 600 EMR/EHR and Practice Management Software companies available in the market, there are many things to consider before using or switching your EMR Software. Practitioners must ensure they have covered every aspect involved before making a final decision. EMR Software or EHR Software (Electronic Medical Records) merely represents maintaining medical records for patients electronically or using a computer system. Specially designed software enables physicians and other medical professionals to store extensive patient data ranging from patient demographics to detailed clinical information, such as medical history, social history, lab reports, etc.
EMR Software by Specialty
Since all medical providers (MDs, DOs, PAs, NPs, LCSW, OT, etc.) work distinctly based on their background and medical specialty, EMR Software or EHR Software must accommodate the unique style and documentation requirements. Examples of such specialty-specific features include the ability to annotate images and store before/after photos for Pain Management and Dermatology specialists, respectively. Similarly, other specialties such as Pediatrics, Oncology, Podiatry, Ophthalmology, Neurology, Nephrology, Dialysis Centers, Rheumatology, and Chiropractic Care require their unique set of specialty-specific features to simplify adoption.
Meaningful-Use
Since the introduction of the HITECH Act, healthcare IT has undergone a massive transition. It started with the transition of the widely recognized Meaningful Use program to what is now known as MACRA, the Medicare EHR Incentive Program. The Meaningful Use program has transformed and is now part of the four components of the new Merit-Based Incentive Payment System (MIPS), which itself is a fundamental part of MACRA.
For some medical practices, the transition from paper-based records to EMR Software (Electronic Medical Records Software) has not been a simple one. Regardless, realizing that the benefits of utilizing ONC Certified EMR Software far outweigh the hassle and challenges associated with it – ensuring a viable future, most practices today have successfully transformed their clinical and administrative operations to EMR Software.
EHR Software Benefits
Aside from ensuring tangible financial incentives and profitability, practices converting to EMR / EHR Software have seen the following benefits:
- Improved Practice Efficiency
- Improved Profitability and Revenue Cycle (Medical Billing Services)
- Patient Engagement(via Patient Portal)
- Decreased Stationary Costs
- Better Care Coordination
- Enhanced Security and Safety (Cloud Storage & Back-ups) – Cloud-based EMR Software
- Connectivity between doctors & hospitals across the country – Health Information Exchange (EMRs with HIE connectivity)
EHR Software Based on Practice Size
Not all EMR Software vendors suit hospitals and clinics with multiple specialties or providers. Similarly, EMR Software vendors designed for larger organizations such as hospitals or multi-provider clinics do not usually support a solo doctor practice or a small medical enterprise. Budgetary constraints aside, many other factors will make an EMR Software vendor viable for your medical practice. From solo-provider clinics to large multi-provider and multi-specialty clinics, every practice has unique inherent challenges that must be addressed by their respective Electronic Medical Records (EMR) Software vendor.
Small or Solo Provider Practices
A small doctor’s office not only has a limited number of staff members but their EMR Software budgets are also meager compared to a large enterprise such as a hospital. Due to these budgetary constraints, many providers simply choose to employ Free EMR Software or choose an affordable EHR Software vendor with a low fixed monthly fee. Cloud-based access is one such important requirement so that these providers can access patient charts even from home when needed.
Large Practices
Larger group practices generally comprise more than fifteen or often twenty medical providers. These practices usually provide medical services that fall under various medical specialties (Orthopedics, Pain Management, Surgery, Chiropractic Medicine, Family Medicine, etc.). Therefore, these practices require support for multiple users to access the system simultaneously and for the Scheduling software to accommodate multiple locations, providers, and resources such as Dialysis Chairs, procedure room allocation, etc. These practices also keep replacing or adding staff members and need a scalable solution.
Medium-Sized Practices
These practices usually consist of 5 to 10 medical providers, often belonging to the same medical specialty. Their requirements are more stringent, and their budget is also considerably large. Aside from specialty-focused requirements (EMR Software by Specialty), these practices also require unique features such as interoperability, dedicated customer support, multi-device support, and an extensive reporting functionality to keep an eye on the overall performance of the practice.
Hospitals or Enterprise Organizations
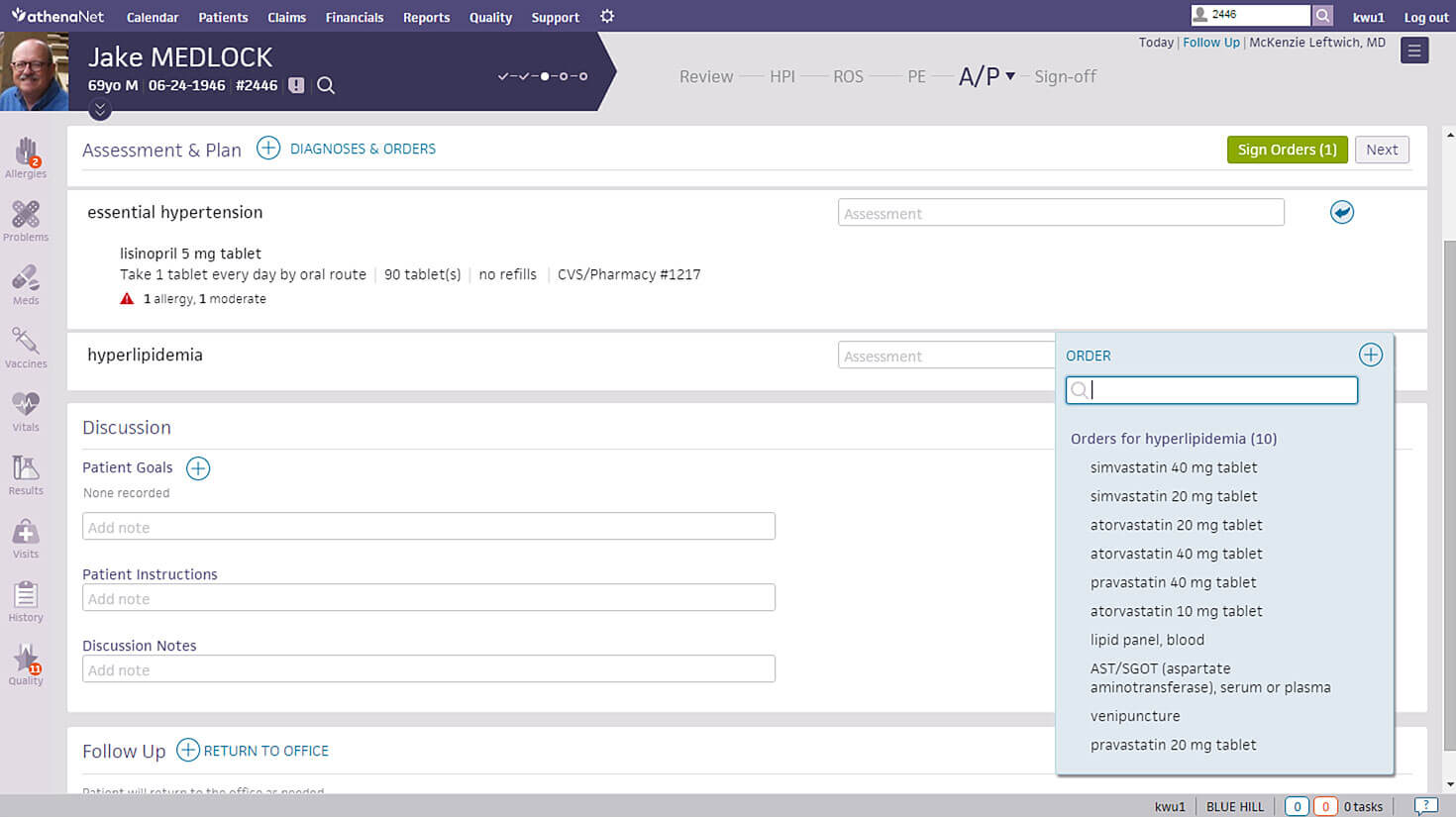
EHR companies such as Epic, Cerner, AllScripts, NextGen, Athenahealth, IMS by Meditab, eClinicalWorks, Meditech, McKesson, MEDHOST, etc., usually target and provide solutions for larger corporations like Hospitals, ACOs, PCMH, IPAs, CINs (Clinically Integrated Networks), Public Health Departments, etc.
These customers have the most elaborate list of requirements, which are usually documented in the form of an RFI or RFP to assess and shortlist vendors that can meet them. The requirements consist of features like inventory management modules, interface with local labs (LIS), machines, and diagnostic equipment along with drug dispensing (Pharmacy Management Software) and Electronic Medication Administration Record (EMAR), etc. These entities also require the EHR Software also need to integrate with multiple other software and medical devices.
Why Does Your Practice Need EMR Software?
Since the introduction of Meaningful Use, most healthcare practices have had little or no choice but to convert their practice operations to an EHR system. However, most providers today select the EHR vendor of their choice that best suits their specific needs and must perform an extensive search to evaluate all available options before they find one that is suitable. Most potential EMR Software buyers in the market today have the following in common:
- Do not know what they are looking for
- Know exactly what they want but don’t know where to start or find it
- Relying on advice from colleagues using EMR software already
Although #3 is ideal, every provider and practice workflow is unique, and therefore what works for one provider may not suit the other. “One size fits all” simply doesn’t apply in the world of healthcare IT. Software experts and industry specialists are an ideal source of information, advice, and ultimately ensuring that the right decision is made.
What To Look For In A Potential EHR Software Vendor
EMRs include several types of software based on specific applications or functionalities:
Cloud-Based EMR Software
Small doctor offices benefit the most from Cloud-based EMR Software technology since minimum to no upfront cost or maintenance is required. Additionally, there is the added benefit of accessing your EHR (Electronic Health Record) software from any device with internet access. This type of software is also device-independent in most cases and can be accessed using devices such as Smartphones (Android & iOS), iPhones, iPads, laptops, and desktop computers. The move to the public cloud for healthcare is vital in the changing landscape. For practices that don’t adopt new cloud services, the old inferior feature set coupled with the higher prices will hinder the business dramatically. This gulf between the old software and the new cloud-based software will only grow more exponentially as time goes on.
Mac EMR Software
Apple dominates the digital devices and computer market in the US today, so it is no surprise that many providers are specifically looking for their EHR Software vendor to support the Mac Operating System (Mac EMR Software). Not all vendors today work on a Mac device, so looking for a vendor with native support for Mac devices is essential to ensure that the software performs on existing hardware at the practice and does not require more investment in computer systems.
EHR Software Essentials
Electronic Health Records (EHR) Software for practices offering specialties should provide tools and templates to reduce the workload of the practice by featuring seamless documentation of the daily clinical workflow of the specialties and specifying the areas of concern. It should also provide improved methods for capturing text, scanning images and reports, e-prescription, and management of raw data.
This is the most significant requirement for most software buyers today as the software must comply with the standards and guidelines set by the Office of the National Coordinator (ONC). The online repository details all software vendors and details related to their respective compliance with the measures set by the ONC (Click here). Software that complies with these standards has undergone rigorous testing and met a benchmark level defined by the federal body. The software testing done during this exercise checks all areas of the EMR Software system from Patient Portal access to the way the EHR Software communicates with other programs and entities like labs, Pharmacies (via e-Rx), hospitals, HIEs, etc.
Integrated Practice Management (PM) Software
With competition rising in healthcare IT, EMR Vendors providing integrated Practice Management (PM) systems as part of their overall software package easily outperform rivals with standalone EHR Software including those that may provide a specialty-specific EHR Solution. EMR Software companies with integrated Practice Management solutions often tend to provide extensive reporting capabilities to track practice performance and manage business operations better.
Integrated Medical Billing Software
Operations within a medical practice can be streamlined by EMR Software. One such important operation is billing for services rendered and communications with insurance companies. Medical Billing Software, therefore, works best when integrated with Electronic Health Records (EHR) Software. All clinical documentation seamlessly conforms to the required standard and forms a financial document that can be electronically sent to payers (insurance carriers) to verify and process at their end. This simplifies the operations and ensures all parties are on the same page when it comes to the financial health of the enterprise. Medical Billing Software helps practices and Medical Billing managers generate claims, and patient statements, verify patient eligibility, and more. This software is ideal for practices that want to handle billing in-house and integrate it with EMRs.
Security
An EMR Software must ensure the safety and security of patient records while ensuring privacy and HIPAA compliance for patient/doctor communication (Patient Portal). This is a paramount concern for physicians and HIPAA compliance should be guaranteed at all times by the EHR Vendor. Most Vendors today (Epic, Cerner, Athenahealth, AdvancedMD, PrognoCIS, Modernizing Medicine, eClincalWorks, etc.) are aware of the importance of HIPAA compliance and have taken steps to ensure the safety of patient records security in every section of the EHR Software using advanced tools like data encryption, to enhance the security of the EMR software.
Athenahealth EHR Software
Specific Services
One of the decisions your practice will have to make is whether you want just an EMR system or one with integrated Practice Management for Medical Billing and Patient Scheduling. There are advantages to having both together but there have been cases where some practices only go for one in case they had unique requirements that a vendor could not fulfill, or they had already paid a hefty amount for a PM system and weren’t looking to replace it yet.
Ease of Use and Training
Doctors are not IT professionals, and though some might be tech-savvy, it would be egregious to expect them all to be experts on EHR software. Ease of use is essential to make the transition from paper to electronic smooth, as well as day-to-day practice to go along without a hitch. If the software is too complicated and hard to understand, it’s a waste of precious time and needlessly aggravating. Some vendors offer free training while others don’t make sure you ask for training when you purchase if your staff needs it.
Specialty-Based EMR Software
Every medical provider works uniquely, thus some EMR Software Vendors today have decided to tailor their EHR Software for a particular specialty or a limited number of specialties. This has been the inevitable culmination of the EHR Software journey, as more and more specialists were required to start using Electronic Medical Records Systems. Since the majority of the EHR Software suppliers at the time were focused on selling to all medical providers regardless of specialty, specialty providers soon learned that their software did not necessarily meet the requirements or their unique clinical workflow. Therefore, the demand for a specialty-specific EMR System gave birth to a specialty-focused EMR Software market. Vendors started introducing specialty-specific EHR Software and today there are unique EMR Systems available for the most demanding specialties such as Oncology, Dermatology, Chiropractic Medicine, Orthopedics, Pain Management, General Surgery, Alternative, and Holistic Medicine, etc.
Customer Support Quality
Your EHR Software may meet all your expectations, but what happens when you encounter an issue? It’s not inevitable for any software application to malfunction or behave unexpectedly from time to time. This is where you must pick up the phone and speak to one of the customer service representatives of your EMR Software Company. A good customer support team can address even your most complex concerns in a knowledgeable and skilled manner, fixing small glitches while you are on the phone. Major issues or changes to the behavior of your Electronic Medical Records application will require not only a knowledgeable customer service rep but one who will go the extra mile and pass on your concerns to the appropriate departments to fix the issue and ensure customer satisfaction. Similarly, a bad agent will just make things worse. Some vendors provide support as a part of the plan you’re already paying for, while others charge extra for support. Scout the market, read reviews, or just ask point blank if there will be a special support team assigned to each practitioner and whether you’ll be charged for the service. Most importantly, however, you must speak to existing users of the EMR Software company to learn about their experience with the customer support team.
Hidden Cost
There are varying price lists out there, some offer free services, while others charge an arm and a leg for specialty services. Either way there will be hidden costs that you might get to know about later. Fix your budget and talk to vendors you interview about hidden costs within the contract and whether services such as training and support are free.
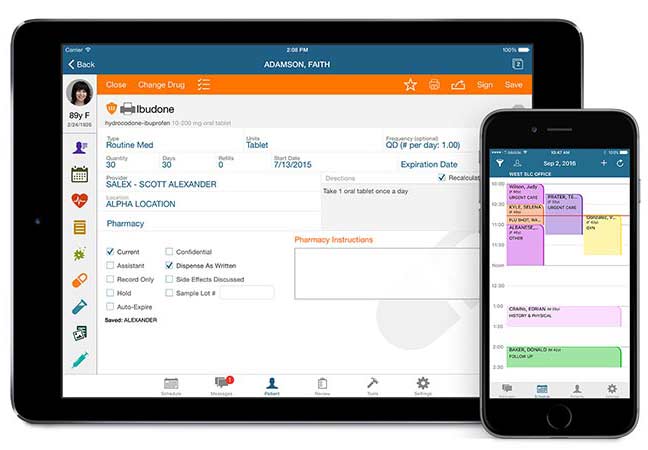
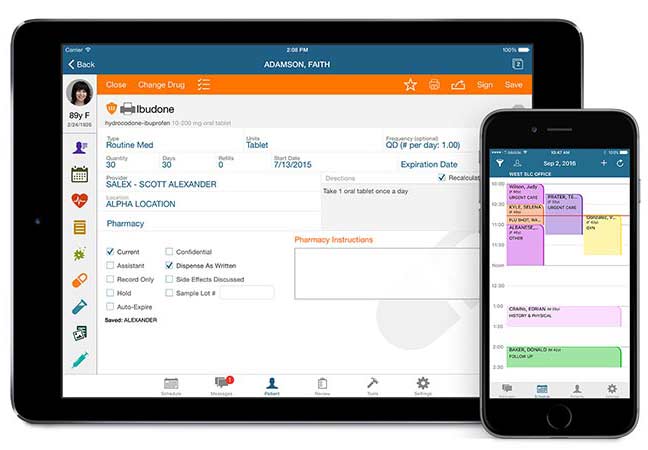
Mobility
Smartphones have changed the dynamics of mobile usage. Handheld devices are easy to carry around and can be used for any number of uses. Most people are ditching the cumbersome PC for a handheld device. Doctors mostly use iPads or Tablets in the examination room to take down patient symptoms, check the history, and note down the prescription, so the vendor must have a mobile application that is synced with all the mobile devices being used in the practice.
AdvancedMD Mac EMR
Market Trends To Be Aware Of
Like anything else, the EMR industry is also subject to changes. From new technology to legalities and governing bodies, everything is constantly changing. Here are some of the changes medical practices should keep track of.
Meaningful Use Changes
At a recent healthcare conference, Andy Slavitt, the administrator of the Centers for Medicare & Medicaid Services, declared that Meaningful Use was over, and would be replaced by the end of this year with something better. But a deeper look into the claims revealed that meaningful use would very much still be there, only much improved.
The new measures aim to make the reporting and benchmark for reaching the required reports much easier and laxer than under Meaningful Use, along with other changes. Yet it is safe to say that none of these changes will make an impact until the end of 2017.
Cloud-Based Services
It’s no surprise that more vendors are switching to Cloud-Based EMR software. Cloud-based EMR software systems can cut down on steep upfront costs that otherwise would be spent on client servers, and they can even be hosted from any device with an internet connection and web browser, making them a much more convenient option. Research has found that only 25% of practitioners are interested in a web-based EMR system, whilst 50% are willing to have it as an initial model that eventually transitions to cloud-based.
Accessibility
The EHR software industry is quickly widening its range of practice types to become accessible to a wider range of healthcare services. The number of people who lack the time and knowledge in health IT is increasing each year. This makes optimizing these EMR software solutions more difficult as they must now cater to different needs. Douglas W. Bowerman, MD, predicts we will see a “continued trend towards accessibility” in Electronic Health Records software, both in terms of how we access them – on mobile, for instance – and who can access the EHR software.
Real-Time Analytics
Medical practices and healthcare facilities generate huge amounts of patient data. This data aids clinicians and medical practitioners in clinical decisions (CDS) and by utilizing analytic algorithms, interoperability-related accessibility issues can also be solved. The development of data warehouses can also provide an opportunity to ensure the accuracy of patient information due to automation.
Blockchain
Most notably used in cryptocurrency and NFTs, blockchain technology has recently found use in Electronic Medical Records software systems. The technology uses cryptography to secure medical record data, ensuring that it can only be viewed by someone with given access. This could even be used for validating information such as clinical trials, and claim results, tracking medicine distribution, and preventing insurance fraud. Starting from early 2022, blockchain technology has already been implemented to secure data and keep confidentiality.
5G
5G networking is set to become a standard of data communication technologies in the next few years. 5G may not be able to completely integrate with health IT software, despite even offering up to 100 times the speed of ordinary 4G networks. There are still many different mediums of data transfer all of which are already competing to standardize EMR software communication. Due to this, many Electronic Health Records software solutions use different communication methods, making them incompatible and unable to communicate with each other. Therefore, despite its promises, 5G networks will not get past this bottleneck until there is an agreed standard.
Standardization
Currently, Electronic Medical Records software systems are regulated by very lax standards. Due to this, some Electronic Health Records software vendors have had to pay millions of dollars in settlement fees, regarding false claims about meaningful use certifications. Regulations, for electronic medical records, are becoming far more strict and more transparent, to prevent such incidents in the future. Medical billing coders will likely use separate interfaces from physicians as they both require unrelated data, so sharing the same regulations would likely lead to life-threatening miscommunication.
Patient-Centered Engagement
The growth of your practice can be benefited greatly by boosting patient engagement. One approach can be to make resources and content readily available within patient communities. Another can be to increase patient outreach. Additionally, regular appointment reminders (which can be handled via appointment reminder EMR software) can reduce cancellations and improve patient engagement.
Changing Dynamics
Electronic Health Records (EHR) Software is constantly influenced by developments in technology. A common example is the recent addition of AI Virtual Assistants to EMR software systems, being able to assist practitioners with daily tasks and increase practice efficiency. With industry leaders such as Apple and Google looking to enter the healthcare space, more competition can be expected between Electronic Medical Records software vendors. This will likely lead to the rapid modernization of EHR solutions and large-scale updates.
Better Patient Access
While better patient access is expected of many EHR software systems, the feature has not been completely integrated yet. According to a study in 2019, only 10% of patients (who had access to their records) viewed them. Additionally, of these patients, 63% were encouraged to do so by their respective providers. Vendors of electronic medical records software (EMR software) are updating their systems to be easier to navigate and to better suit patients’ requirements; this also prepares EMR systems for potential future regulatory changes. More health practices are also providing more guidance and raising awareness to encourage more patients to regularly check their health records before appointments.
EHR Footprint
Electronic Health Records software systems must be inclusive of a wide range of digital capabilities. By working towards better data liquidity, data would be more accessible and therefore increase the EHR footprint – which can be done without compromising on security. Additionally implementing interoperable electronic health record systems (EHR systems) would also allow better access and exchange of patient information between healthcare organizations.
Digital Therapeutics
Digital therapeutic software uses different methods to help treat patients and medical conditions. It is typically used via mobile devices (i.e. smartphones and tablets) and is beginning to integrate into Electronic Medical Records software systems and become more patient-centric. The popularity of digital therapeutics can only be expected to rise as they start to meet industry requirements and clinical trials continue to be published.
Reducing Errors
While many electronic medical records software systems facilitate better accuracy and efficiency, human error is not completely eradicated. Error prevention is something that is not currently addressed properly in EMR and EHR software. In previous years, it was common to blame handwriting for inaccurate paper prescriptions – however, even with computers, relying too much on them can be dangerous. In one instance, a 16-year-old patient was prescribed 38 tablets of medicine (in 2013), which resulted in an overdose. Currently, Electronic Medical Records (EMR) Software developers are developing solutions, such as decluttering physician notification centers to allow more time to be spent with patients and reduce distractions.
Searchability
Presently with Electronic Health Records software systems, being able to easily process large amounts of data can prove to be quite a hassle. Current generations of EMR systems still seem behind and dated in terms of UI and ease of use. However, this is beginning to change as more EMR vendors have begun providing updated UI in their EHR software solutions to facilitate easier data access to electronic health records.
Wearable Devices
Wearable devices have been popular in the medical industry, with the market still expected to grow by 26.8% from 2022 to 2028. By improving the accessibility of healthcare metrics (for both patients and practitioners), diagnosis has become much more simplified. Additionally, by integrating this data with Electronic Medical Records (EMR) software systems, there is the potential to innovate patient healthcare and health IT solutions. The technology is currently compatible with specialized health apps on mobile phones, smartwatches, and fitness trackers.
Easy Access
Patients require quick, easy, and secure access to their data so that they can be engaged and informed in their healthcare. The Electronic Medical Records (EMR) software industry is evolving with the latest health IT technology to improve on these points, which will help patients build better trust with their providers. This trend will likely continue, for greater health outcomes.
Widespread Interoperability
There’s a lack of data-sharing standards across EMR software systems, which stops patient information from being shared across different practices. This can lead to problems in diagnosis (for patients who visit various centers) and even for the patients themselves. To solve this, EHR vendors are adding more updates to their software to make Electronic Medical Records software more interoperable. And to include more integrations to allow such data to be shared more efficiently.
Patient Portal
There are many benefits to a patient portal EMR system. They remove the need for paperwork and manual fetching of data, and they offer a direct portal for patients to view their medical records. By allowing easy access to their records, patient portals also encourage patients to be more involved in their healthcare, which also enables easier diagnosis for medical practitioners.
Artificial Intelligence (AI)
Artificial intelligence and machine learning have both had major impacts on health IT in recent years. It is likely that as these continue to evolve and change, they will have just as big of an impact on EMR software systems. AI and machine learning algorithms can improve Electronic Health Records software by making them more intuitive and efficient. They can help streamline medical workflows and help improve patient outcomes. Applying these technologies to EHR software systems can also enable physicians to provide much more personalized and proactive care, by identifying any potential health issues early through analysis of patient data. By providing access and insights into large amounts of patient data, artificial intelligence, and machine learning algorithms have the potential to revolutionize clinical research and drug development.
Latest Updates In EHR Software
Get Ready For The New Generation Of EMR Software
Advancements in the fields of Artificial Intelligence and Analytics have induced a boom in the Healthcare IT industry. EMR Systems and Practice Management Software are becoming highly optimized and increasingly robust giving birth to a newer generation of EMR Software. Don Woodlock in an article for HealthcareITNews claims that the benefits of this new generation include reduced costs, improved flexibility, and customization of EHR Software.
Physician Burnout: A Global Problem
Adam C. Uzialko in Business.com talks about how Electronic Medical Records (EMR) Software helps reduce healthcare burnout. Burnouts are becoming more and more common in the healthcare industry and are becoming a great concern. Medical Software such as EMR Software and Practice Management Software helps optimize workflows and reduce stress and burnout. Healthcare IT Software like telemedicine EMR Software also helps in reducing work stress and improving physicians’ work efficiency.
Cybersecurity
As we progress into 2024, cybersecurity in Electronic Medical Record (EMR) systems is set to become increasingly sophisticated in response to rising cyber threats. Key developments will include advanced encryption and the use of blockchain for enhanced data integrity. Artificial Intelligence (AI) will be crucial for real-time threat detection and predictive analytics, and compliance with global data protection regulations will become more critical, necessitating adaptive strategies from EHR providers. Additionally, user training will gain prominence to mitigate risks associated with human error. Overall, the focus will shift towards building a proactive, resilient digital healthcare environment, fortified against emerging cyber challenges.
Customization
Heading into 2024 and beyond, the EMR (Electronic Medical Records) software trend is gravitating toward increased customization and modular design. The diverse and evolving needs of healthcare providers across various specialties drive this shift. Customizable EMR systems will allow medical professionals to tailor interfaces and functionalities to their specific workflows, enhancing efficiency and reducing cognitive load. Modular EMR systems will offer flexibility, enabling healthcare facilities to integrate only the modules they need, such as telemedicine, billing, or patient engagement tools, thereby avoiding the complexities of one-size-fits-all solutions. This approach improves user satisfaction and facilitates better patient care by providing clinicians with tools that align with their practice needs. Ultimately, this evolution will lead to more adaptable, efficient, and user-friendly EMR systems in the healthcare industry.
Public Health
As we get closer to the digital healthcare era, the use of EMR systems in public health is becoming more and more crucial. EMR systems are essential for improving disease surveillance and management since they give real-time access to patient data in a variety of healthcare settings. EMRs are predicted to be essential tools for monitoring public health trends in the future, allowing medical professionals to quickly recognize and address new health emergencies like epidemics or patterns of non-communicable diseases. They make it easier to gather and analyze vast amounts of health data, which is necessary for developing policies and making well-informed decisions on public health. EMRs also help with the effective distribution of resources and the evaluation of public health interventions’ efficacy. EMR systems are crucial in forming a proactive and data-driven approach to public health because they function as a bridge between individual patient care and population health management.
Healthcare Costs and Efficiency
EMR software’s ability to lower healthcare costs and increase efficiency is becoming increasingly clear as we move deeper into the digital healthcare era. Clinical workflows are predicted to be greatly streamlined by EHR software by 2024 and beyond, saving a substantial amount of time and money on administrative duties. Its effectiveness allows medical professionals to concentrate more on patient care rather than paperwork, resulting in cost savings for healthcare facilities. Effective treatment plans and preventive care strategies can be developed at a lower cost by utilizing the advanced data analytics capabilities of EHR software. To further reduce costs, it is projected that integrating EMR software with other digital health tools will reduce the number of redundant tests and procedures. EMR software has the potential to play a major role in advancing the development of a healthcare system that is both more effective and affordable.
Global Adoption and Localization
As the healthcare industry progresses globally, the adoption and localization of EMR systems are becoming key factors in transforming healthcare delivery. In 2024 and onwards, a significant trend will be the customization of EMR systems to meet the specific needs of different regions and countries. This includes adapting to various languages, cultural norms, and legal requirements, ensuring that EMR systems are not only universally accessible but also relevant to local healthcare contexts. In developing regions, EMRs are expected to leapfrog traditional healthcare infrastructure challenges, offering an efficient way to manage patient data and improve healthcare delivery. The localization will also involve integrating region-specific medical practices and protocols into EMR systems, enhancing their utility and acceptance among healthcare providers. This global adoption, coupled with thoughtful localization, is crucial for creating a more interconnected and efficient global healthcare system, where patient data can be seamlessly exchanged across borders, leading to improved health outcomes worldwide.
Mobile Health
As we advance into 2024, the synergy between mobile health and Electronic Medical Record (EMR) accessibility is set to redefine healthcare delivery. The proliferation of smartphones and mobile devices has paved the way for mobile health apps that seamlessly integrate with EMR systems, enabling patients to access their health records, schedule appointments, and communicate with healthcare providers from anywhere. This mobile accessibility is crucial for enhancing patient engagement and empowerment, promoting transparency in healthcare services. For healthcare providers, mobile Electronic Health Records (EHR) access facilitates the delivery of care outside traditional settings, supports decision-making with real-time data, and enhances coordination among care teams. This integration is also vital in remote and underserved areas, where mobile solutions can bridge gaps in healthcare access. Moving forward, the continued evolution of mobile health coupled with EMR accessibility will play a pivotal role in making healthcare more patient-centered, efficient, and accessible globally.
Emerging Technologies
As we move forward into 2024 and beyond, the integration of EMR systems with emerging technologies is poised to revolutionize the healthcare sector. Advanced technologies like Artificial Intelligence (AI), machine learning, and blockchain are increasingly being incorporated into EMR systems to enhance their capabilities. AI and machine learning algorithms are being used for predictive analytics, improving diagnostic accuracy, and personalizing patient care plans. Blockchain technology is emerging as a key player in securing EMR data, ensuring tamper-proof records, and enhancing patient privacy. Additionally, the integration of Internet of Medical Things (IoMT) devices is facilitating real-time health monitoring and data collection, directly feeding into EMR systems for more comprehensive patient profiles. These technological integrations not only promise to streamline healthcare operations but also aim to significantly improve patient outcomes by providing more accurate, efficient, and secure healthcare services.
Sustainability and Green IT
As the healthcare industry continues to evolve into 2024 and beyond, the focus on sustainability and Green IT in the context of Electronic Medical Record (EMR) systems is gaining unprecedented momentum. The integration of sustainable practices and green technologies within EMR infrastructures is not only aimed at reducing the environmental footprint of healthcare IT operations but also at enhancing system efficiency and reducing operational costs. Energy-efficient data centers, cloud-based services, and virtualization are becoming key components in making EMR systems more eco-friendly. These technologies help minimize the energy consumption and carbon emissions associated with the storage and processing of vast amounts of medical data. Additionally, the push towards digital records over paper significantly reduces waste and resource use. As the industry moves forward, the adoption of Green IT practices in EMR systems will be crucial in achieving a sustainable, cost-effective, and environmentally responsible healthcare sector.
Ethical Considerations
As we advance into the future, ethical considerations surrounding the use of Electronic Health Record (EHR) systems are becoming increasingly critical. The confidentiality and privacy of patient information stand at the forefront of these concerns, demanding stringent security measures to protect sensitive data from unauthorized access and breaches. In addition to privacy, there is a growing emphasis on equity and fairness in EMR accessibility, ensuring that all patients, regardless of socio-economic status or geographical location, benefit equally from the technological advancements in healthcare. Furthermore, the integrity of patient information raises ethical questions about the accuracy and completeness of records, highlighting the importance of maintaining high standards in data entry and management. Ethical use of EHR also encompasses the responsible application of predictive analytics and AI, ensuring that these technologies do not introduce bias or compromise patient care. As the healthcare sector continues to embrace digital transformation, navigating these ethical challenges with a patient-centered approach will be paramount in fostering trust and delivering equitable, high-quality care.
Precision Medicine and Genomics Integration
As the medical field progresses, the integration of precision medicine and genomics into healthcare practices is becoming increasingly vital. Precision medicine’s aim to tailor treatment and prevention strategies to individual genetic profiles is revolutionizing patient care. This personalized approach is heavily reliant on the integration of genomic data into Electronic Health Record (EHR) systems, allowing for seamless access to patient genetic information by healthcare providers. Such integration facilitates the identification of genetic predispositions to diseases, enabling earlier and more targeted interventions. Furthermore, it supports the development of customized treatment plans that are more effective and have fewer side effects. The ethical management of this sensitive genetic data, ensuring privacy and informed consent, remains a paramount concern. As we move forward, the fusion of precision medicine and genomics with digital health records promises to enhance the effectiveness of healthcare delivery, making it more personalized, predictive, and preventive.
Cross-Sector Data Integration for Holistic Health
As healthcare systems evolve, the concept of cross-sector data integration is becoming increasingly essential for achieving holistic health outcomes. Integrating data from diverse sectors such as healthcare, social services, and environmental agencies into Electronic Health Record (EHR) systems enables a more comprehensive understanding of the factors influencing individual and community health. This holistic approach facilitates the identification of social determinants of health, such as socioeconomic status, education, and living conditions, which are crucial for tailoring preventive and therapeutic interventions. The challenge lies in developing interoperable systems that can seamlessly exchange data while maintaining strict privacy and security standards. As we move forward, leveraging big data analytics and AI will be key in synthesizing these vast datasets to provide actionable insights. Embracing this cross-sectoral data integration will not only enhance patient care but also foster a proactive, preventive healthcare model that addresses all facets of health determinants.
Enhanced Data Security and Privacy
As we navigate deeper into the digital era, enhancing data security and privacy within healthcare systems, particularly in Electronic Medical Record (EMR) platforms, has emerged as a paramount concern. The surge in digital health data necessitates robust security measures to protect sensitive patient information from cyber threats and breaches. Innovations in encryption technologies and the adoption of blockchain are pivotal in fortifying EMR systems against unauthorized access, ensuring that patient records are both secure and tamper-proof. Furthermore, stringent adherence to data protection regulations, such as HIPAA in the United States, reinforces the legal framework for privacy and security. Educating healthcare professionals on best practices for data handling and implementing advanced user authentication mechanisms are critical steps in mitigating risks. As healthcare continues to embrace technology, prioritizing data security and privacy will be essential in maintaining patient trust and upholding the integrity of healthcare delivery.
Natural Language Processing (NLP)
Natural Language Processing (NLP) is playing an increasingly vital role in enhancing Electronic Medical Records (EMR) systems by improving how healthcare providers interact with digital records. By enabling computers to understand and interpret human language, NLP facilitates more efficient documentation processes, allowing clinicians to dictate notes and automatically convert them into structured data. This technology reduces the administrative burden on healthcare professionals and minimizes the risk of errors associated with manual data entry. NLP also allows EMR systems to extract valuable insights from unstructured data, such as clinical notes and patient narratives, helping providers identify trends and make more informed decisions. Moreover, NLP algorithms can assist in coding and billing processes by accurately interpreting medical terms and procedures, ensuring compliance with regulatory standards.
NYC Consolidates Its EHR Systems Onto One Epic Platform
Epic EHR Software rolled out a new H2O system (Health + Hospitals Online) in Brooklyn at one hospital and 10 community health centers including NYC Health + Hospitals and neighborhood uniting 40,000+ users and 70+ patent care facilities on a single platform. EMR Software features decision support tools, Revenue Cycle features, and a Patient Portal.
Latest in Pathology EMR Software
As of 2023, pathology Electronic Medical Record (EMR) software has seen significant advancements, driven by technological innovations and evolving healthcare needs. In 2021, the FDA approved the first AI-based digital pathology system, Paige Prostate, which integrates with EMR platforms to diagnose prostate cancer, marking a milestone in AI adoption in pathology. This approval accelerated the integration of AI and machine learning into pathology EMR systems, enabling features like automated image analysis and predictive diagnostics.
In 2022, the adoption of cloud-based pathology EMR solutions surged, with companies like Proscia and PathAI launching platforms that offer scalable, secure, and collaborative environments for pathologists. These systems facilitate real-time data sharing and remote diagnostics, which became critical during the COVID-19 pandemic.
Additionally, the rise of whole-slide imaging (WSI) technology, which gained FDA approval for primary diagnosis in 2017, has been increasingly integrated into EMR systems, allowing pathologists to digitize and analyze slides remotely. Interoperability improvements, driven by the 21st Century Cures Act (2020), have also pushed vendors to ensure seamless data exchange between pathology EMRs, LIS, and hospital EMRs.
Furthermore, in 2023, major EMR software providers like Epic and Cerner expanded their pathology modules to include advanced analytics and customizable reporting, addressing the growing demand for data-driven insights in diagnostic workflows. These developments highlight the ongoing transformation of pathology EMR software into a more efficient, accurate, and collaborative tool for modern healthcare.